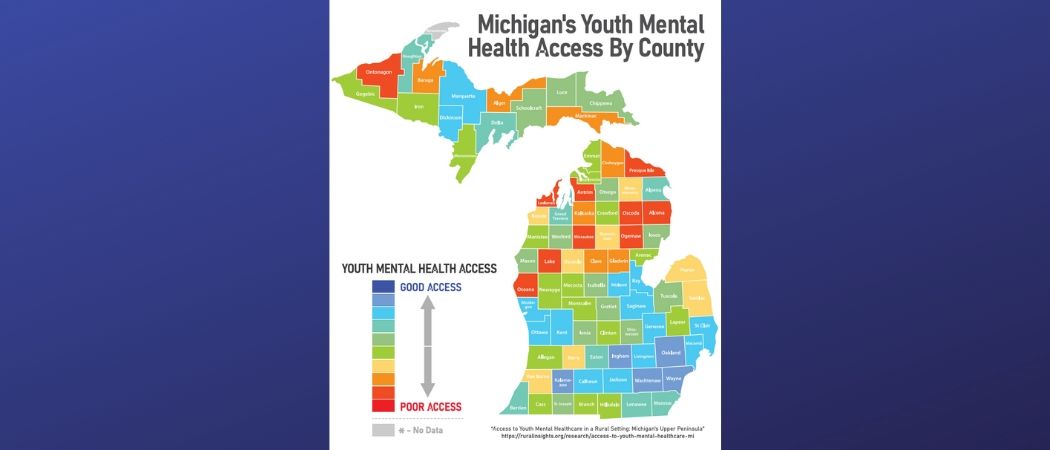
Access to Youth Mental Health Care in a Rural Setting: Michigan’s Upper Peninsula
ABSTRACT
The number of children and youth committing or attempting suicide is on the rise in a dramatic and disturbing way. Officially, suicide is the second leading cause of death among youth age 15-24, and for every suicide death among this population, there may be as many as 100 to 200 suicide attempts (Youth.gov). Depression and anxiety is commonplace for people under 18, and is often a stepping stone for more severe mental health diagnoses continuing on into adulthood if left unaddressed. Although it is common for individuals to experience temporary emotional distress as they progress through childhood, rates of mental health diagnoses are alarming and for a variety of reasons, children are not receiving the mental health services that they need in order to live healthy and productive lives. In the case of the Upper Peninsula of Michigan, known as the “U.P.,” the problem is only intensified by geography. Its rural nature creates added barriers to accessing mental health care, exacerbating a national shortage of physicians and psychiatrists further, where only one child psychiatrist serves the entire Upper Peninsula. There are no inpatient beds for children who experience serious mental illnesses, and instead, they are driven up to 9 hours away from home to a facility either in Grand Rapids or Green Bay. The financial costs of mental health care can prove to be too heavy a burden for Medicaid carriers, private insurance carriers, and especially the uninsured.
According to the Office of Adolescent Health (2018), access to care generally includes three components; (1) gaining entry into the healthcare system, usually through insurance coverage (2) accessing a location where needed health care services are provided, based on geographic availability, and (3) finding a health care provider whom the patient trusts and can communicate with. As examined in this report, Michigan’s Upper Peninsula lacks adequacy in all 3 areas of access.
Poor mental health and mental illness have profound effects on communities, families, and the individual. As citizens and neighbors, the Upper Peninsula must take action towards improving the lives of those who are the future of this country. Mental health has been difficult to quantify as compared to physical health, but its effects are felt increasingly and with more regularity in youth populations. If we demand an equal opportunity to seek care for visible illnesses, we must also address the invisible ones that take the lives of children daily. Health care providers and the State of Michigan must take steps to alleviate the burden of accessing mental health care for youth, as mental health is linked to overall happiness and prosperity within a society. If we allow our youth to fail, our society will fail; we must step up for our children.